Solving the Vaccine Puzzle
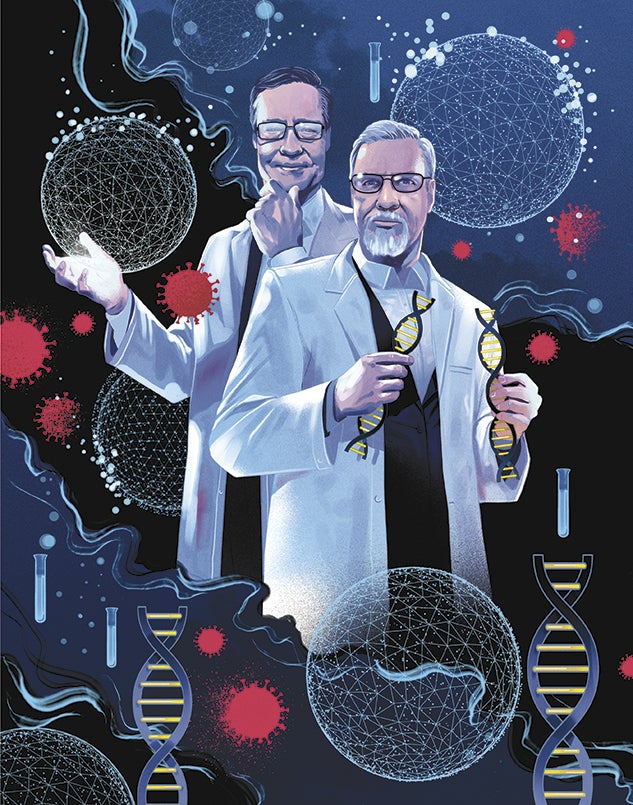
Former roommates and careerlong colleagues Barney Graham and Bill Gruber have been instrumental in the development of vaccines for respiratory diseases and HIV. Today, they’re at the forefront of the COVID-19 pandemic — working to piece together lifesaving vaccines in record time.
By Cindy George
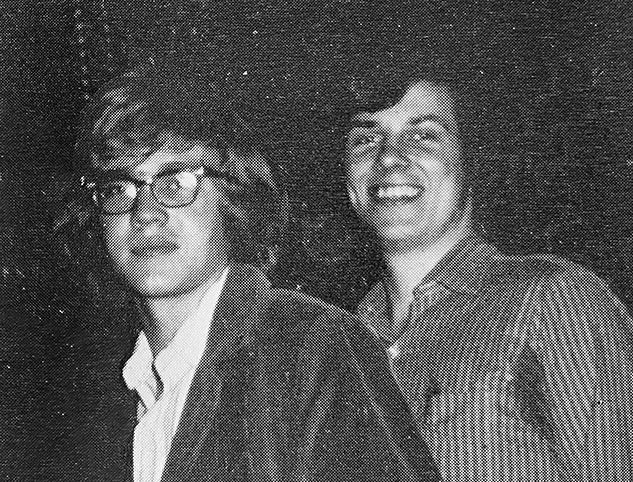
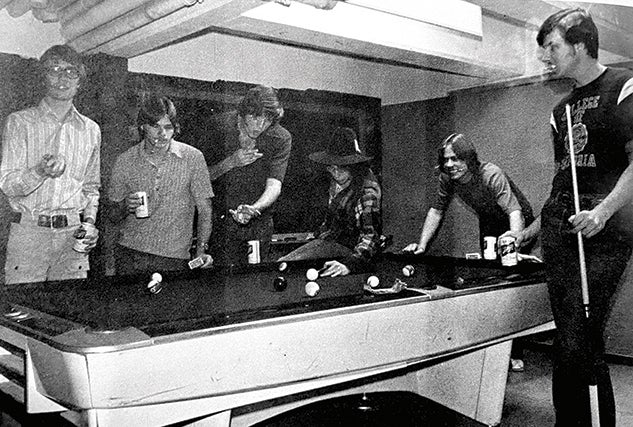
Barney S. Graham and William C. “Bill” Gruber met in 1971 as Rice freshmen. Graham, a farm boy from Kansas, and Gruber, from what was then the outskirts of Houston, became podmates and fast friends in Will Rice College before graduating in 1975.
Over the next half-century, both earned medical degrees and became physician-researchers focused on infectious diseases with careers that tracked with science and serendipity. Despite decades as emblems of excellence — working in elite arenas on difficult problems — both now find themselves sharing what may be the most urgent challenge of their professional lives: COVID-19, the global public health crisis.
Having enjoyed a five-decade friendship of mutual admiration, they now are also colleague competitors. Graham, from his lab at the National Institutes of Health (NIH), and Gruber, as a global executive for the pharmaceutical behemoth Pfizer, are at the forefront of the race for a vaccine to control SARS-CoV-2, the novel coronavirus that causes COVID-19. “We’re solving for a pandemic situation,” Gruber said. “We’re talking about condensing a process that typically takes sometimes a decade into months.”
They share the weight of an awesome responsibility. SARS-CoV-2, which emerged in late 2019, has now claimed the lives of at least 355,000 people in the United States and over 1.8 million worldwide while sickening millions more.
We’re solving for a pandemic situation. We’re talking about condensing a process that typically takes sometimes a decade into months. — Bill Gruber '75
At the time of this story, Graham’s NIH vaccine with manufacturer Moderna and Gruber’s Pfizer vaccine in partnership with the German biotechnology company BioNTech were competing to be the first to market. In November, each company released preliminary data suggesting that its vaccine was more than 90% effective in Phase 3 clinical trials. By mid-December, both vaccines had received emergency use authorization from the FDA. That placed the pandemic’s end on an emptying hourglass.
“Even though Moderna started first on March 16, we were just getting to Phase 3 July 27,” Graham said in a joint conversation with Gruber. “I just want to remind Bill that Pfizer also started Phase 3 July 27, but we started in the morning and they started in the afternoon.”
Gruber shot back with a chuckle. “There’s still a little competitive spirit here,” he said.
Academic Origins
According to Graham, he and Gruber began as undergrads on dissimilar academic footing.
“I got into Rice early decision during my junior year of high school. It was the only place I ever applied to college. I just really wanted to go to a relatively small school in a warm climate,” said Graham, who came from the tiny town of Paola, Kansas. When his admissions interviewer asked what books he’d read the previous summer, Graham said none, explaining that he’d built a barn with his brother and managed a farm with pigs, cows and horses.
I was pretty far behind my whole freshman year, and if it wasn’t for Bill, I probably wouldn’t be doing what I’m doing right now. — Barney Graham '75
“I was pretty far behind my whole freshman year, and if it wasn’t for Bill, I probably wouldn’t be doing what I’m doing right now,” said Graham, whose deep voice has a deliberative pace. “I saw how Bill worked and how he studied, and I saw what was possible, so I really just buckled down. After that first semester, I think I almost got all A’s, but it was because I was trying to catch up with Bill.”
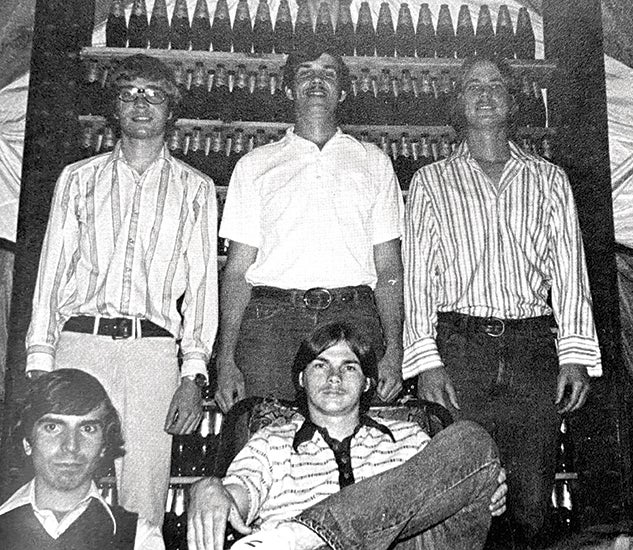
Gruber grew up in Houston’s Spring Branch area. Well-prepared for the rigor of college, he had applied to several schools. “In the end, Rice was just the thing that was going to work out best for me,” he said.
After graduation, Graham went to medical school at Kansas University, his parents’ alma mater, while Gruber headed across the street from Rice to Baylor College of Medicine. Graham became an internist while Gruber chose pediatrics. But each — unbeknownst to the other — became intensely focused on infectious disease research.
Career Collisions
In 1986, they bumped into each other at a conference. Their science posters ended up being displayed side by side. Graham was at Vanderbilt University in Nashville and Gruber was working at Baylor College of Medicine and Texas Children’s Hospital.
“We just couldn’t believe it. We were both working in the same field, in the same area of interest in terms of a respiratory pathogen, respiratory syncytial virus (RSV) that affects children and adults,” said Gruber, who speeds through his sentences like a sprinter. RSV is the single most important cause of pediatric hospitalization in the U.S., with 40,000–120,000 infant hospitalizations each year. It is a major reason for infant morbidity and mortality throughout the world.
We just couldn’t believe it. We were both working in the same field, in the same area of interest in terms of a respiratory pathogen, respiratory syncytial virus (RSV) that affects children and adults. — Bill Gruber '75
“Barney was telling everyone about all the cool stuff happening in Nashville, and I developed a great deal of envy. … I actually got back to my office and was kind of lamenting. And literally, on the top of my stack of mail that had gathered while I was gone was a solicitation for the position that Barney was talking about with the pediatric infectious disease group. And so, I applied. Lucky for me, they accepted me.”

Over the next decade, Graham and Gruber authored a few papers together at Vanderbilt on RSV, but in 1999, Gruber left for a job in industry.
“He went to Wyeth on the premise that he was going to go to a place where he could actually make antiviral vaccines that could be used in somebody’s arm and really get out there and make a difference,” Graham said. “I was pretty much doing mouse experiments, trying to understand the immunology of RSV and mostly T-cell biology and things that were not really of a lot of interest to industry. But, Bill, you know, he wanted to turn his virology and vaccinology expertise into something practical, to actually make products.”
In 2000, Graham, who by then had earned his Ph.D. in microbiology and immunology, left Vanderbilt to join the NIH. He was recruited to help develop an HIV vaccine clinic and work in a new vaccine research center at the National Institute of Allergy and Infectious Diseases (NIAID), led then and now by the famed infectious disease expert Anthony Fauci.
Fundamental Breakthrough
The foundational work of Graham and collaborators on RSV set a new course for vaccine development by decoding the structure of the “prefusion” F protein, which controls the entry of a virus into a host cell. The most potent neutralizing antibodies attach to the prefusion F, which shape shifts into a “postfusion” form after pulling the virus and host membranes together to infect the cell.
“Finding that shape and conformation of the protein before it rearranges turned out to be more important than just getting the structure,” Graham said. Gruber said not knowing enough about the prefusion structure contributed to the difficulty in developing vaccines, as did preventing the F protein’s postfusion form, which is less immunogenic and less likely to produce a good antibody response.
The foundational work of Graham and collaborators on RSV set a new course for vaccine development by decoding the structure of the “prefusion” F protein, which controls the entry of a virus into a host cell.
“That work was fundamental,” Gruber said.
The breakthrough was published in 2013. Graham was eager to discuss the advancement with Gruber at a scientific meeting that October. Then, the federal government shut down. Unable to travel for work, Graham and his wife decided to leave their Maryland home and take a road trip.
“I’ve never seen the leaves in the northeastern part of the country during October,” Graham said, adding that he could skip the chaos of a conference and spend time talking to his old friend. The Grahams stopped to see friends in Philadelphia, New York City, New Hampshire and, specifically, Gruber and his wife in Warwick, New York. After pleasantries and a Mediterranean meal, the vaccine scientists retreated to Gruber’s study.
“The time with Bill was special because there’s not three people on Earth who really want to talk about the F protein of RSV,” Graham said. “I think it’s very exciting and it just isn’t something you can talk about with everybody.”
The time with Bill was special because there’s not three people on Earth who really want to talk about the F protein of RSV. I think it’s very exciting and it just isn’t something you can talk about with everybody. — Barney Graham '75
Soon after, Gruber, who had joined Pfizer when the company bought Wyeth in 2009, took a team to meet with Graham and his group to set up a license agreement to acquire the stabilized form of the F protein. Pfizer scientists further stabilized the structure to create a new vaccine for pregnant women to protect their babies from RSV that has reached Phase 3 clinical trials.

COVID-19 Emerges
Graham’s RSV work became the gateway to understanding coronaviruses such as MERS-CoV, which causes the Middle East Respiratory Syndrome first identified in 2012, and led his lab to work with messenger RNA (mRNA) company Moderna on a potential vaccine for that virus and anything new.
“We were partnering with them because that manufacturing technology is fast, and we had a protein design that we thought could work, so if there was a new coronavirus outbreak, we would be ready to jump on that, which we did,” said Graham, who is now deputy director of NIAID’s Dale and Betty Bumpers Vaccine Research Center and chief of the institute’s Viral Pathogenesis Laboratory.
Because Pfizer was already working with mRNA company BioNTech on an influenza vaccine, they too were ready to fast-track development of an mRNA-based COVID-19 vaccine.
Before this year, no mRNA vaccines for infectious disease had been approved for human use, which makes first-to-market COVID-19 vaccines using this technology a dual breakthrough.
In November, The Atlantic’s Sarah Zhang described the “triumphant” accomplishment this way: “If mRNA vaccines help end the pandemic and restore normal life, they may also usher in a new era for vaccine development.”
Before this year, no mRNA vaccines for infectious disease had been approved for human use, which makes first-to-market COVID-19 vaccines using this technology a dual breakthrough.
Relying on mRNA technology, the Pfizer-BioNTech and Moderna-NIH COVID-19 vaccines under development now hold promise for safe administration, rapid production and low manufacturing costs. Unlike traditional vaccines, those produced with mRNA don’t require injecting a virus into the patient to produce antibodies. Instead, mRNA molecules trick the cells into making proteins and reproducing antibodies with no virus present — and with the immune system reacting in an authentic way.
“They started manufacturing based on the sequence we thought would produce a stabilized spike protein using their mRNA delivery almost immediately — within three days of Jan. 10, when the [SARS-CoV-2] coronavirus sequence was released,” Graham said. “And so, we got off to a very quick start, and that’s why we had the first Phase 1 clinical trial that opened up March 16.”
Vaccine scientist Peter Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine and co-director of the Texas Children’s Hospital Center for Vaccine Development, said vaccines are “our most effective lifesaving interventions” and heaped praise on both Graham and Gruber.
“Both of these individuals have made monumental contributions to vaccine science, and the hope is that their work will lead to new innovations not only for COVID-19, but for a variety of different virus vaccines,” he said. Hotez, a fellow in disease and poverty at Rice’s Baker Institute for Public Policy who also serves as a Rice adjunct professor in biomedical engineering, noted Graham as a “pioneer in viral immunology and vaccine development.”
Both of these individuals have made monumental contributions to vaccine science, and the hope is that their work will lead to new innovations not only for COVID-19, but for a variety of different virus vaccines. — Peter Hotez

A Vaccine Race
The COVID-19 puzzle has been “all-consuming” since Jan. 7, 2020, Graham said, when a prototype for a pandemic preparedness demonstration project turned into real life. Graham and Gruber, both 67, said they have never worked so hard. The Pfizer-BioNTech and Moderna-NIH formulations are two-dose vaccines. Hundreds of millions of doses will be needed immediately — and, eventually, billions.
“We need more than one company to be successful, because I think no single company is going to be able to produce vaccine doses as fast as needed to quell the epidemic,” said Gruber, who is now senior vice president of Pfizer Vaccine Clinical Research and Development, responsible for the company’s global clinical development of vaccines. Many challenges remain — in supply chain, cold storage, access for low-wealth countries and public trust — for uptake of the vaccine.
We’ll eventually convert this to an endemic disease that doesn’t have the impact it has now. That’s the goal. We need more than two vaccines to be successful here because we’ve got a lot of people to vaccinate. — Bill Gruber '75
“The Pfizer vaccine is going to have to be kept frozen — at least for transport for any sort of extended period of time. It can be kept in the refrigerator for several days after it’s thawed,” Gruber said. Graham said the Moderna product has to be frozen as well, but can remain at room temperature for 30 days after being thawed.
Both companies will be seeking more stable formulations for use in low-income and middle-income countries. There’s no guarantee that whatever vaccinations are produced will provide durable protection for years to come; they may have to be updated and administered annually like flu inoculations.
“We’ll eventually convert this to an endemic disease that doesn’t have the impact it has now. That’s the goal,” Gruber said. “We need more than two vaccines to be successful here because we’ve got a lot of people to vaccinate.”
Despite the whirlwind they endured in 2020, both scientists feel grateful to have the knowledge, experience and energy to face the challenge.
“When this first happened, I considered myself among the fortunate few in that I can actually try to do something about this, as opposed to sort of waiting and hoping that something happens. That, in many ways, is empowering,” Gruber said. “I’m hopeful that we can convey some sense of reassurance for the public that, yes, something is coming. Help is coming.”
WEB EXTRA: In October, the combined homecoming, reunion and Families Weekend featured a special President’s Lecture Series event with former Will Rice roommates Barney Graham ’75 and Bill Gruber ’75, both leaders in two of the first COVID-19 vaccines. Graham, deputy director of the National Institute of Allergy and Infectious Diseases’ Vaccine Research Center, and Gruber, senior vice president of Pfizer Vaccine Clinical Research and Development, shared stories from their years at Rice and their oft-intersecting careers in medicine, research and vaccine development.
Watch and listen to their conversation here.