Real-Time Evolution
Bacteria’s growing resistance to antibiotics is a looming public health crisis. Rice researchers in Yousif Shamoo’s lab are conducting experiments to discover how to slow the rapid evolution of bacterial resistance.
According to the Centers for Disease Control and Prevention, at least 2 million people in the United States fall ill due to antibiotic-resistant infections each year. Of those people, at least 23,000 die.
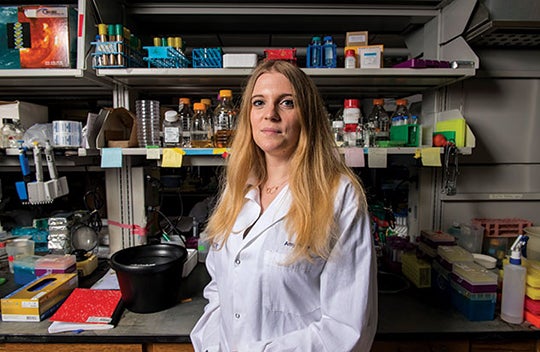
Amy Prater, a doctoral student in biochemistry and cell biology, is researching ways to address this growing health care challenge by revealing the underlying biological pathways that enable bacteria to evolve resistance. This, in turn, could lead to the development of new treatments to delay the emergence of resistance. She’s part of a group of postdocs and graduate and undergraduate students in the lab of Yousif Shamoo, professor of biochemistry and cell biology and vice provost for research.
Prater works with a species of bacteria called Enterococcus faecium, which naturally inhabits the gut and mouth of humans. “But if you have a weakened immune system, like if you have HIV/AIDS or are undergoing chemotherapy, those bacteria can become very dangerous,” she said.
This and similar bacterial species are naturally less susceptible to antibiotics like penicillin that attack their cell walls. Prater looks at how these unusually tough bacteria adapt to the “last resort” drug, daptomycin.
Prater’s experiments start with growing mucuslike biofilms of E. faecium in a container called a bioreactor. Each day, she adds just enough daptomycin to make cells with resistance traits much more likely to survive and reproduce than other cells. She takes samples from her bioreactor each day to see which bacterial genes contain mutations and how common they are. This “bacterial evolution” takes 10–30 days.
“If we can understand how that resistance is evolved [and] identify the molecular and physical mechanisms that confer that resistance, eventually we could develop tandem co-drugs that could be administered along with antibiotics to delay the onset of that resistance,” Prater said.
Essentially, this means sick patients might one day take a combination of an antibiotic and a “resistance inhibitor” that would keep the bacteria in their body from adapting so quickly. This way, the lifetimes of current antibiotics may be extended.